A Spotlight on ME/CFS

Every human being has experienced fatigue – we all know how it feels to be tired. A tough day at work, a strenuous workout at the gym, a long study session, a sleepless night consoling a sick child, or a day of running endless errands prompts the need for an extended period of rest. In these situations, some relaxation and a good night’s sleep are usually the best remedies. You wake up feeling refreshed and energized, ready to tackle the challenges in the days ahead. For countless individuals, this is not the case. Imagine that you did not have the ability to carry on with your normal daily routine due to profound exhaustion. What if you were unable to tolerate simple tasks such as taking a shower, getting dressed or even engaging in a conversation? This is the reality for millions of people who have a disease called myalgic encephalomyelitis (ME), commonly known as chronic fatigue syndrome (CFS).
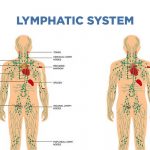
Myalgic encephalomyelitis is a serious medical condition with an estimated 20 million people who have received a diagnosis and more than 90% of people yet to be diagnosed. According to the Centers for Disease Control (CDC), it is estimated to be up to four times more common in women and typically develops between the ages of 40 and 60. Prior to the onset of the illness, some people develop a sore throat or swollen lymph nodes. Although no single cause has been identified, the CDC has cited viral infections as potential triggers (e.g. Epstein-Barr virus – EBV, human herpesvirus- HHV). While the presence of a virus may be a key factor in some cases, it does not paint a complete picture of the etiology. Physical or emotional trauma, genetics, and environmental factors, e.g. toxin exposure, may also play a role.
ME/CFS involves a complex constellation of symptoms which compromise health and quality of life. Among the top three issues reported by most patients are severe fatigue, widespread muscle and joint pain, and unrefreshing sleep. Additionally, patients may experience cognitive disturbances, gastrointestinal issues, bladder conditions, sexual dysfunction, headaches/migraines, orthostatic intolerance (intolerance to upright positions) and sensitivities to sound, light, touch, and chemicals. Many patients also contend with brain fog, which is described as a decline in cognition with respect to focus, concentration, and processing information. These problems significantly interfere with function and disrupt daily routines, contributing to isolation.
While ME/CFS is most prevalent in adults, it can strike at any age. It has been noted that ME/CFS has developed in children after the flu or mononucleosis. There are many negative developmental, emotional and functional consequences that occur when the condition emerges during childhood, as its effects will impact educational and social interactions. Diagnosing younger individuals can be more challenging as they may not be able to clearly describe their symptoms. In these cases, parents play a critical role in helping the physician to identify changes in the child’s behavior and activity level. Symptoms in children and adolescents are similar to those experienced by adults, however, orthostatic issues, headaches, and stomach pain are the most common complaints.
There are various conditions that are often concurrent in patients with ME/CFS which complicate diagnosis and treatment. Some examples include fibromyalgia (a non-inflammatory condition characterized by widespread musculoskeletal pain and fatigue), Ehlers-Danlos syndrome (EDS – a connective tissue disorder that affects the joints, skin and blood vessels), Sjogren’s syndrome (an autoimmune condition that involves many different symptoms including dry eyes and mouth, fatigue and joint pain), postural orthostatic tachycardia syndrome (POTS – a form of dysautonomia which causes pooling of the blood in the legs, limiting tolerance to upright positions), neurally mediated hypotension (a condition in which a sudden drop in blood pressure causes nausea, dizziness and sometimes fainting) and mast cell activation syndrome (a disorder which causes an exaggerated immune response due to overactive mast cells). As these issues can occur separately from ME/CFS, their individual complexity warrants additional discussion.
One of the perplexing features of ME/CFS that distinguishes it from other chronic illnesses is what is known as post-exertional malaise (PEM), more recently called post-exertional neuroimmune exhaustion (PENE). The way in which a typical person recovers from activity is vastly different than the manner in which an individual with ME/CFS copes with exertion. PEM is the hallmark sign of this condition and is required to make the diagnosis. Following any amount of physical, mental, or emotional effort, individuals may experience flu-like symptoms, severe pain and fatigue, sleep disturbances, and changes in cognitive function. All of these issues require reduced activity and prevent the individual from engaging in his or her normal routine. The exacerbation of symptoms may occur immediately following activity or may be delayed by several hours or days and the recovery period may extend to weeks or even months. The implications of PEM on exercise will be discussed in a separate article.
The presentation of ME/CFS is highly variable. Some people are able to maintain independent function while as many as 25% become homebound or even bedridden, requiring full-time care. The economic burden of this disease calls for thoughtful consideration concerning social and financial support. The inability to work affects many individuals, which impacts not only the family unit but also destabilizes the community. Disability coverage may be denied due to misdiagnosis or lack thereof. The characterization of fatigue as the primary feature of this illness has done a great disservice to patients, drastically minimizing the magnitude of their suffering. The pervasive misunderstanding of the disease has narrowed the channels of access to resources which has contributed to the hardship that all patients face.
The process of diagnosis remains elusive in part due to the variability of case definitions. The diagnostic criteria have been revised by a number of different committees over the course of the past several decades, marked by the publication of the Holmes case definition of CFS in 1988. In 1991, the Oxford Criteria was established based on the results of studies funded by antidepressant manufacturers and psychiatrists. The issue with these criteria was that PEM was not listed as a symptom and certain psychological disorders such as anxiety and depression were not excluded. This meant that the patient population in clinical studies was more heterogeneous, skewing the results upon which the criteria were based.
While the 1994 Fukuda Criteria which has long been used as a diagnostic guide did list PEM as a symptom, it was criticized as it did not require it for diagnosis. In contrast, the Canadian Consensus Criteria (CCC) from 2003 focused on PEM as a cardinal sign of the disease. Feedback from clinicians indicated that the CCC criteria were too complex to implement in busy clinical settings, leading to the publication of the International Consensus Criteria (ICC) in 2011 as a result of the collaboration of twenty-five experts. Modifications included the new label of PENE and the elimination of the 6-month time frame which was previously required for diagnosis.
Chronic fatigue immune dysfunction syndrome (CFIDS) and post-viral fatigue syndrome (PVFS) are among the other names for ME/CFS. This represents inconsistencies with regard to its identity in the literature and in the clinical setting. The CFS label is very misleading as it fails to paint an accurate picture of the factors that contribute to debility. In 2015, a committee was commissioned by multiple government agencies to redefine the illness. The expert panel suggested a name change to systemic exertion intolerance disease (SEID) to highlight the multi-system presentation and the significance of post-exertional malaise. Their efforts served to dispel myths about the disease, encouraging the necessary shift in its classification from a psychological to a physiological illness. The release of this Institute of Medicine (IOM) report demanded that the government prioritize funding for research.
The timeline that outlines the history of the disease’s discovery and variable classifications is marked by the changing political climate and the associated responses of regulatory organizations. Evidence of ME/CFS was first described in the 1930s as a form of atypical polio. A subsequent outbreak of unclear origin occurred in 1955 amongst staff at the Royal Free Hospital in London. Despite the fact that nearly 300 patients shared the same symptoms, the condition was described by the media as a case of mass hysteria. Dr. Melvin Ramsey later coined the term myalgic encephalomyelitis which helped to minimize the psychological connotation associated with the disease.
History repeated itself in 1984 when a cluster of cases surfaced around the region of Incline Village, Nevada. Following an investigation by the CDC, the case was closed without resolution, leaving hundreds of patients invalidated and without proper care. The 1988 CDC report gave rise to the term chronic fatigue syndrome, which contributed to the ignorance about the true nature of the condition. At that time, the media’s portrayal of the epidemic as the ‘yuppie flu’ further downplayed the seriousness of the problem. The term CFS has been tied to a long history of stigmatization perpetuated by political agendas which have contributed to inadequate care. Although the ME/CFS label remains the most widely used to date, some authorities have suggested that there are subsets of patients whose clinical presentation may not be justified by either name.
As there is no known cure for ME/CFS, physicians have been focused on symptom alleviation and management. In the absence of an FDA approved medication regimen, some physicians have prescribed antiviral medicines as well as off-label use of specific drugs including Rituxan (Rituximab), Methylphenidate (Ritalin), and Ampligen (Rintatolimod). While Rituxan has been approved to treat autoimmune conditions such as rheumatoid arthritis and certain forms of cancer, there are potentially serious side effects, some of which may be permanent. While some patients have experienced benefits, its efficacy has been equivocal for patients with ME/CFS as it has not been proven successful in clinical trials.
Interestingly, some patients have also been treated with Methylphenidate, the drug that is commonly prescribed to treat ADD (attention deficit disorder) and ADHD (attention deficit hyperactivity disorder). A 2016 study concluded that use over a four week period was effective in roughly 1 in 3 patients with ME/CFS who had concentration issues. It is important to note that the majority of participants in this study were middle-aged females and that the dosage and frequency of the medication intake were variable as assessed by a questionnaire.
Even with its success in clinical trials, Ampligen is only available in the United States on a limited basis without insurance coverage and is accessible only under special circumstances in Europe due to its experimental status. Despite the fact that many patients have attested to its life-altering effects, its use remains limited due to its extreme cost. Although it was approved in Argentina in 2016, it remains largely out of reach for most patients. The Hunter-Hopkins Center in North Carolina opened by Dr. Charles Lapp in 1995 is one of the only facilities in the United States that is FDA approved to administer Ampligen.
As one of the few doctors with many years of experience treating ME/CFS, Dr. Lapp made others aware of the consequences that patients suffer due to the widespread lack of knowledge in the medical community. His decision to name his center after two of his patients reflected his dedication to his profession. In addition to his years as a treating physician, he also served as an educator. His teachings focused on the importance of palliative medications, the key role of supplements in symptom reduction, and the functional applications of exercise. In a 2018 interview, he spoke about his desire to stay involved with the ME/CFS community despite his retirement, with the hope of developing a web-based accredited education program.
In the past several years, there have been a number of eye-opening documentaries that have brought attention to ME/CFS. Unrest, featuring and directed by Jennifer Brea, offers an enlightening portrayal of her battle with the disease. In this film as well as during her TED talk, she delivers a powerful account of her journey. As a newly engaged Ph.D. student at Harvard with a bright future ahead, she suddenly became ill and her symptoms became progressively worse. When medical testing failed to provide a clear answer, she was told that she had conversion disorder – that she was displaying this illness as a result of a distant trauma that she may not even recall. Her physicians insisted that it was all in her head. She emphasizes how the devastation of her experience was compounded by her doctors’ disbelief of her illness.
Historically referred to as neurasthenia, women who were suffering from symptoms similar to those that afflict today’s patients with ME/CFS were frequently admitted to institutions with a diagnosis of hysteria. Throughout the course of time, there have been a number of diseases that were regarded as mental illnesses before diagnostic tests existed to prove otherwise. Prime examples of this are the early references of multiple sclerosis as ‘hysterical paralysis’ and the institutionalization of patients with epilepsy. Even in the past decade, there have been instances in which patients have been forcibly removed from their homes and sent to a facility to receive psychiatric care. Perhaps the most well-publicized case of this scenario is that of Karina Hansen of Denmark. This remains a charged issue and one which has implored increased attention from the medical community.
While such extreme actions have not been documented in the United States, the undertone of doubt about the illness greatly undermines the care that patients receive. Prior to the deterioration of her health, Jennifer had developed a fever from which she never fully recovered. This is a common occurrence in many patients that precipitates the development of the disease. Physicians have recognized that many patients with ME/CFS are in fact able to identify a specific point in time at which their health changed, seemingly correlated with the presence of an infection or virus which preceded their decline. This critical piece of information can facilitate a more expeditious diagnosis which would spare patients a great deal of time and frustration as they seek relief. Sharing her personal experiences has allowed Jennifer to utilize her suffering to connect with other patients with ME/CFS, giving them the opportunity to tell their stories. As co-founder of the ME Action Network, she has played an integral role in raising consciousness worldwide.
The standards of care have gradually improved as people have continued to speak out, resulting in the development of specialized treatment centers across the country. One such facility is the Whittemore Peterson Institute, which was founded in 2005 by Annette and Harvey Whittemore on behalf of their daughter, Andrea. Their mission, along with Andrea’s physician, Dr. Daniel Peterson, was to create an organization dedicated to providing education and supporting research to pave the way for treatment and a cure. While they have worked to accomplish this goal, the establishment has not been without controversy. There were various scientists associated with the institute whose discoveries with regard to the viral mechanisms that underlie ME/CFS became the focus of great dispute. Dr. Judy Mikovits was a lead researcher who along with her team called attention to XMRV (xenotropic murine leukemia virus related-virus), a retrovirus thought to be associated with the pathophysiology of ME/CFS.
In 2009, a contentious debate ensued due to contradictory results from follow-up XMRV studies conducted by the National Institutes of Health (NIH) and the CDC. The government later funded a multi-million dollar double-blind study led by a virologist, Dr. Ian Lipkin, who concluded that the results did not statistically confirm the presence of XMRV in patients with ME/CFS or in healthy controls. Dr. Mikovits was subsequently fired and was forced to serve jail time, which destroyed the credibility of her research and her reputation. The book, Plague, details the devastating impact of this dissension on her personal and professional life. The facts surrounding XMRV remain a controversial topic that has furthered the divide within the scientific and medical communities.
The documentary What About ME? expands on the story behind XMRV and highlights the ways in which politics and the media are deeply intertwined in the web where ethics and public policy intersect. In-depth interviews with patients, researchers, physicians, and governmental leaders offer a global perspective that is extremely thought-provoking. Forgotten Plague is another documentary that speaks to the variability of individual experiences and showcases the displacement of patients who are diagnosed with ME/CFS. The film centers around its main director, Ryan Prior, whose life came to a screeching halt during his college years after he developed the condition. His budding career in journalism offered him a platform to champion those who have been forgotten. While giving voice to individual cases including his own, he chronicles the history of the disease and offers insight about the role that politics has played in research and medicine.
As a result of a surge in advocacy, society only recently began to validate ME/CFS as a legitimate medical condition. In 2016, many patients came together worldwide to speak out against marginalization. Led by the ME Action Network, this global campaign became known as the #Millions Missing movement. The protests by patients and families highlighted the inequities they face within the medical system, inspiring an international call to action. Carol Head, President of the Solve ME/CFS Initiative, is also a patient with ME/CFS who has participated in this movement. Carol appeared before Congress in 2017 along with Jennifer Brea and Dr. Zaher Nahle to lobby for the government to solidify its commitment to funding. The subsequent response by the NIH has bolstered intensified research efforts.
Uncovering the physiological components of ME/CFS has been paramount in shifting the medical model to a systems biology approach, which views the disease in a holistic framework. Great strides have been made over the past several years in the areas of immunology (the study of the immune system), genomics (the study of genetics which includes DNA analysis), and metabolomics (the study of metabolites, the chemicals in the blood and other bodily fluids). Groundbreaking research is fostering a greater understanding of the underlying mechanisms involved in ME/CFS.
So how do all of the puzzle pieces fit together? Studies have revealed that ME/CFS is hypometabolic in nature, meaning that individuals who are diagnosed with it lack some of the fundamental building blocks that drive normal metabolic function. In addition, research has elucidated the complex interaction between the brain and associated organs, specifically the hypothalamic-pituitary-adrenal axis (HPA axis) and the role of the immune-inflammatory response.
With so many scientists engaged in cutting-edge research, the Open Medicine Foundation (OMF) has provided a collaborative space for the exchange of information. The organization was founded in 2012 by Linda Tannenbaum, whose daughter has ME/CFS. The OMF has spearheaded the End ME/CFS Movement, raising over $8 million for research. The process of unraveling the tangled threads of the disease is indeed complicated and has required focus from many different scientific specialties. The pace of research has picked up in the past few years thanks to a considerable amount of private funding, further reinforced by several impassioned leaders whose family members are also battling the illness.
Dr. Ronald Davis, a renowned geneticist and inventor in California, stands at the forefront of the movement to discover a cure for ME/CFS. His tireless efforts have been fueled by the plight of his own son, Whitney Dafoe, who has become an invalid as a result of the disease. Whitney’s case is truly astounding, shedding light not only on the depth of his suffering but also on that which is experienced by his family members, whose lives have been permanently altered. The focus of Dr. Davis’ research is on understanding the nature of metabolic deficiencies at the cellular level and uncovering specific biomarkers in order to develop non-invasive or less invasive testing measures.
One of the pioneers of autoimmune disease research is Dr. Nancy Klimas. Her revolutionary insights concerning the role of inflammation and cytotoxicity were responsible for generating interest for future studies in this area. Her enthusiastic pursuit of knowledge dates back to the 1980s, at which time she was one of the few clinicians who studied ME/CFS. In her work as a professor and as the Director of the Institute for Neuroimmune Medicine at Nova Southeastern University in Florida, she remains devoted to enhancing the lives of her patients while continuing to test the boundaries of science. Her current research is focused on gender differences in patients with ME/CFS as well as determining biomarkers in female patients.
Since founding the Bateman Horne Center (BHC) in 2015, Dr. Lucinda Bateman has continued her crusade for improved patient care. Her original non-profit organization known as OFFER (Organization for Fatigue and Fibromyalgia Education and Research) along with her Fatigue Consultation Clinic evolved into the BHC with the support of multiple private donations. The BHC has been acclaimed as a center for excellence, offering clinically focused, compassionate care to patients with chronic diseases.
Dr. Bateman’s dedication has supported her goals to expand research and extend the reach of professional and patient education. In 2018, she hosted the first annual roundtable meeting which brought together eleven doctors from across the country who have developed expertise in diagnosing and treating patients with ME/CFS. This gathering created a forum for clinical leaders to discuss their treatment approaches and has set the benchmark for continued research.
Another trailblazer who has dedicated his time to improving the quality of medical care for patients with ME/CFS is Dr. Jose Montoya. As head of the Stanford University ME/CFS Initiative, he has presented many case studies in great detail and has encouraged his colleagues to exercise greater discernment and precision with regard to patient assessment and treatment. His specialty in infectious diseases has allowed him to gain a better understanding of the nuances of ME/CFS symptoms. All of these physicians have elevated the state of patient care while demonstrating a passionate commitment to healing.
With a focus on the topic of brain inflammation, Dr. Jared Younger has conducted studies that have strengthened the claim that ME/CFS is a neuroinflammatory disease. His goal is to produce a safe, non-invasive diagnostic test to measure brain inflammation which would serve as clinical confirmation of this issue. Dr. Mark Davis is an expert immunologist who has been instrumental in identifying the role of T cells (thymus cells) in the immunological reactions that occur in ME/CFS. Neuroscientist Dr. Alan Light along with his wife, Kathleen, have focused on the role of genetic mutations in the expression of pain and fatigue. Dr. Maureen Hanson and Dr. Robert Naviaux have shared the results of their studies pertaining to metabolism. They have looked specifically at the changes in the function of mitochondria, the energy producing components of the cells.
The concept of a metabolic trap is a hypothesis that has required unique attention. Although the details are beyond the scope of this article, it is important to mention this idea. Dr. Robert Phair, the founder of Integrative Bioinformatics, has been donating his time to work alongside the Stanford team. Through his combined training in electrical engineering and physiology, he has offered a fresh perspective on this topic. By studying data from patients who have the most severe form of the disease, he has identified common genetic mutations that affect metabolism. The hope is that this information will shed more light on the underlying causes of the disease in all patients.
While there is no way to adequately credit every individual who has contributed to the research on ME/CFS, these acknowledgments provide an overview of the scientific efforts in the United States. There are studies of equal importance being conducted throughout the world, such as the research of Dr. Jonas Bergquist in Sweden. His work has focused on determining cellular level changes in proteins and hormones which better explain the underlying pathophysiology of PEM and the associated neuro-inflammation. Translational research has been conducted by Dr. Oystein Fluge, an oncologist in Norway, along with his colleague, Professor Olav Mella, in an effort to better comprehend the disease process and links between ME/CFS and cancer.
As researchers continue to uncover the mystery of ME/CFS, additional clues about its mechanisms are being revealed. Scientists are stepping closer to a cure as they continue to push the envelope. At a recent conference in Sweden, Dr. Zaher Nahle presented a comprehensive lecture detailing the state of research and medicine, noting the triumphs that have resulted from advocacy efforts and the various scientific and clinical advances that have been made in the recent years. In recognition of the need to expedite research, the NIH funded a five-year collaborative project at three facilities which include Cornell University, Columbia University, and the Jackson Laboratory in Connecticut. This action honored the needs of patients across the globe and will be crucial to support continued scientific exploration.
Fortunately, new diagnostic tools are being developed that will allow doctors to understand the various ways in which the disease manifests. The nanoneedle was created by Dr. Ronald Davis and his colleagues to facilitate the process of diagnosis. This innovative chip is capable of analyzing a small drop of blood to assess energy production. It will play a pivotal role in distinguishing the differences between healthy cells versus those from patients with ME/CFS. Scientists also intend to use it to identify specific biomarkers that will clarify the pathogenic imprint of the disease. Its applications are especially promising as it is extremely cost effective to manufacture and implement.
Although science has come a long way, there is undoubtedly much more work to be done. Perhaps the greatest challenge faced by the medical field at large is the gap between research and clinical practice. What is the most pragmatic way to disseminate information so that medical professionals can apply this knowledge to patient care? What can be done to help patients thrive rather than simply survive? Without immediate solutions, suffering persists while the quest for answers continues. Undoubtedly, there is much more work to be done.
Living with ME/CFS is an unpredictable journey that requires a great deal of courage and resilience from its sufferers. As patients bravely forge ahead, a strong partnership must be maintained between the government and the medical community in order for research to continue. Hope is on the horizon as scientists continue to work fervently to discover a cure. In the meantime, a bright light has been cast that will continue to shine until this dream is realized.
References:
Books:
http://www.plaguethebook.com/
Journal Articles and Online Publications:
A “Metabolic Trap” for Chronic Fatigue Syndrome
https://www.healthrising.org/blog/2018/04/03/a-metabolic-trap-for-chronic-fatigue-syndrome-me-cfs/
An ME/CFS and FM Pioneer Says Goodbye: The Charles-Lapp Interview
https://www.healthrising.org/blog/2018/03/28/lapp-chronic-fatigue-syndrome-fibromyalgia-pioneer-retires/
Ampligen for Chronic Fatigue Syndrome – Still Not FDA Approved (Sept 2018)
https://www.verywellhealth.com/profile-of-ampligen-for-chronic-fatigue-syndrome-716071
Case Definitions for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. BMJ Open. Brurberg et al, Jan 2014.
Chronic Fatigue Syndrome: A Working Case Definition. Annals of Internal Medicine. Holmes et al, 1988.
http://www.ncf-net.org/patents/pdf/Holmes_Definition.pdf
Chronic Fatigue Syndrome: Case Definitions and Diagnostic Assessment. New York State Psychologist. Williams et al, 2014.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5008849/pdf/nihms781173.pdf
Does Methylphenidate Reduce the Symptoms of Chronic Fatigue Syndrome? The American Journal of Medicine. Blockmans et al, Feb 2006.
https://www.amjmed.com/article/S0002-9343(05)00656-X/pdf
Hemispherx to Distribute Second Lot of Ampligen for Use in Multiple Indications in Argentina, the United States and Europe (Sept 2018)
https://www.cmocro.com/news_detail/Hemispherx+to+Distribute+Second+Lot+of+Ampligen+for+Use+in+M/318878/index.html
How To: Diagnosing Chronic Fatigue Syndrome. Health Rising
https://www.healthrising.org/forums/resources/how-to-diagnosing-chronic-fatigue-syndrome-me-cfs.475/
Initiating Care of a Patient with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Frontiers in Pediatrics. Lapp, C., Jan 2019
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6357921/pdf/fped-06-00415.pdf
Leading Chronic Fatigue Syndrome Charities & Organizations (Sept 2017)
https://www.verywellhealth.com/leading-chronic-fatigue-syndrome-charities-and-organizations-4146457
Long Term Methylphenidate Intake in Chronic Fatigue Syndrome. International Journal of Clinical and Laboratory Medicine. Blockmans, D & Persoons, P. June 2016. *ABSTRACT
https://www.tandfonline.com/doi/full/10.1080/17843286.2016.1200816?src=recsys
ME/CFS Collaborative Research Centers and Data Management Center Announcement (Sept 2017)
http://microbediscovery.org/2017/09/27/mecfs-collaborative-research-centers-data-management-center-announcements/
Millions are Missing: Will the World Finally Notice? (Dec 2017)
https://www.huffingtonpost.com/maureen-hanson/millions-are-missing-will-the-world-finally-notice_b_12184042.html
$9.4M NIH Grant Funds Chronic Fatigue Syndrome Center (Sept 2017)
http://news.cornell.edu/stories/2017/09/94m-nih-grant-funds-chronic-fatigue-syndrome-center
Norwegian Rituximab Chronic Fatigue Syndrome (ME/CFS) Trial Fails
http://simmaronresearch.com/2017/11/norwegian-rituximab-chronic-fatigue-syndrome-mecfs-trial-fails/
Plague: An Interview with Dr. Judy Mikovits (June 2014)
https://www.prohealth.com/library/plague-an-interview-with-judy-mikovits-32911
The Puzzle Solver – A Researcher Changes Course to Help His Son (2016)
http://stanmed.stanford.edu/2016spring/the-puzzle-solver.html
The Scientist, the Seahorse and the Nanoneedle – Catching Up with Ron Davis on ME/CFS (June 2017)
https://www.healthrising.org/?s=The++Scientist%2C+the+Seahorse+and+the+Nanoneedle
Reports:
Institute of Medicine (IOM)
Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness. (Feb 10th, 2015)
http://nationalacademies.org/hmd/Reports/2015/ME-CFS.aspx
National Institutes of Health (NIH)
Pathways to Prevention (Dec 1-2, 2014)
https://prevention.nih.gov/sites/default/files/documents/programs/mecfs/ODP-P2P-MECFS-FinalReport.pdf
Interviews, Lectures & Meetings:
Congressional Briefing on ME/CFS (May 2017)
https://www.youtube.com/watch?v=Najd5O7usnQ
Dr. Lucinda Bateman (MD, Bateman Horne Center Founder and Medical Director)
Dr. Bateman’s Summary of Clinician’s Summit March 2-3, 2018 (March 2018)
https://www.youtube.com/watch?v=2w-06T9oAZ8
Global Report of Progress in the ME/CFS Field (Nov 2016)
https://www.youtube.com/watch?v=7pGkAvvEoGA
New Clinical Definitions for ME/CFS (March 2015)
https://www.youtube.com/watch?v=X4Tnt2d-5S8
Dr. Jonas Bergquist (MD, Ph.D., Full Chair Professor in Analytical Chemistry and Neurochemistry in Dept. of Chemistry at Uppsala University, Sweden; Adjunct Professor in Pathology at Utah School of Medicine; Distinguished Professor in Precision Medicine at Binzhou Medical University, China)
The Neuroimmune Route in ME/CFS (Nov 2018)
https://www.youtube.com/watch?v=oXCEJxOmuAY&t=32s
Dr. Mark Davis (Ph.D., Immunologist, Director of the Stanford Institute of Immunology,
Transplantation and Infection)
Research Update (June 2018)
https://www.youtube.com/watch?v=toMhBUZ2dtE
Dr. Ronald Davis (Ph.D., Professor of Biochemistry & Genetics, Stanford University School of Medicine, Director of the Stanford Genome Technology Center)
Biomarkers (Nov 2018)
https://www.youtube.com/watch?v=W11GdwrmZVI
What’s Next? (Nov 2018)
https://www.youtube.com/watch?v=pFzOrknOylA
Research Presentation at the 2018 IIMED Conference (Sept 2018)
https://www.youtube.com/watch?v=WmI5Ri0V51U&t=2341s
An Update on ME/CFS Research (Feb 2017)
https://www.youtube.com/watch?v=sGBXXlQO49g
Dr. Oystein Fluge (MD, Ph.D., Professor, Dept of Clinical Science, University of Bergen, Norway)
Keynote Address: Clinical Trials and Metabolic Features of ME/CFS (Nov 2018)
https://www.youtube.com/watch?v=FKkWb4PsL_8
Dr. Maureen Hanson (Ph.D., Professor – Department of Molecular Biology and Genetics, Cornell University)
Metabolism & ME/CFS – Open Medicine Foundation (Nov 2018)
https://www.youtube.com/watch?v=hPAzInLeSx4&t=1098s
Dr. Nancy Klimas (Director of the Institute of Neuro Immune Medicine at Nova Southern University in Florida)
Discovery Forum 2017: Presentation (Aug 2018)
https://www.youtube.com/watch?v=vEsPWuNNMuU&t=44s
Discovery Forum 2017: An Interview with Dr. Nancy Klimas (Jan 2018)
https://www.youtube.com/watch?v=Aw6ESBGDi5c
Dr. Charles Lapp (MD, Internal Medicine/Pediatrics, Founder Hunter-Hopkins Center, North Carolina)
An Overview of ME/CFS Diagnosis and Management (May 2017)
https://www.youtube.com/watch?v=RTzfWs6Fhl4
Dr. Alan Light (Ph.D. Neuroscientist & Professor at University of Utah School of Medicine)
Genetic Mutations in ME/CFS (Dec 2018)
https://www.youtube.com/watch?v=MqYmvPfqFg0&t=9s
Possible Causes of ME/CFS Pain & Fatigue (Sept 2017)
https://www.youtube.com/watch?v=xDQL7v4XlRU
Dr. Jose Montoya (MD, head of ME/CFS Initiative, Stanford University)
Chronic Fatigue Syndrome: An Unfolding Story of Scientific Discoveries and Fully Targeted Treatments (Feb 2018)
https://www.youtube.com/watch?v=ADVQvzXwDUg
Stanford’s Dr. Jose Montoya on Chronic Fatigue Syndrome (March 2011)
https://www.youtube.com/watch?v=Riybtt6SChU&t=7s
Dr. Zaher Nahle (Ph.D., MPA, current CEO of the Arthritis National Research Foundation, former VP for Research and Chief Scientific Officer for Solve ME/CFS Initiative),
Advances in ME/CFS Research USA (October 2018)
https://www.youtube.com/watch?v=sTQhQf06e-4&t=1148s
Dr. Robert Naviaux (MD, Ph.D., Professor of Medicine, Pediatrics and Pathology, UCSD)
ME/CFS Cell Danger Response, Metabolic Features, Low-Energy in Nature (Sept 2017)
https://www.youtube.com/watch?v=u028TAyB9S4
Dr. Robert Phair (Ph.D., biological systems engineer, Co-founder & CSO Integrative Bioinformatics, Inc)
Metabolic Traps: A New Way to Think About ME/CFS
https://www.youtube.com/watch?v=uej1LXzRbnY
Dr. Jared Younger (Ph.D., Director Neuroinflammation, Pain and Fatigue Lab at University of Alabama, Birmingham)
ME/CFS Involves Brain Inflammation (Dec 2018)
https://www.youtube.com/watch?v=rxdzaWD5wfU
How Brain Inflammation Causes ME/CFS (Nov 2018)
https://www.youtube.com/watch?v=8XrdSlpUQTE&t=87s
Institute of Medicine – Public Release Report Meeting
Committee on the Diagnostic Criteria for ME/CFS (Feb 2015)
https://www.youtube.com/watch?v=Uj1l-tmkRvw
Open Medicine Foundation (OMF)
OMF Worldwide Tour, NY Linda Tannenbaum (Nov 1st, 2017)
https://www.youtube.com/watch?v=Uul2HCWhIF4
Documentaries & Personal Stories:
Forgotten Plague (2015) Directed by Ryan Prior & Nicole Castillo
Unrest (2017) Directed by Jennifer Brea
Invisible Illness – Stories of Chronic Fatigue Syndrome (2015)
https://www.youtube.com/watch?v=9_HwOUiImvw
TED Talk- What Happens When You Have A Disease Doctors Can’t Diagnose – Jennifer Brea (2017)
https://www.youtube.com/watch?v=Fb3yp4uJhq0
What About ME? (2017) Directed by Susan Douglas
Resources:
Action for ME – United Kingdom
https://www.actionforme.org.uk/
Bateman Horne Center
https://batemanhornecenter.org
Centers for Disease Control – ME/CFS
https://www.cdc.gov/me-cfs/
Dysautonomia International
http://www.dysautonomiainternational.org
Ehlers-Danlos Syndrome
https://rarediseases.org/rare-diseases/ehlers-danlos-syndrome/
Fighting Fatigue
http://www.fightingfatigue.org
Health Rising – Finding Answers for ME/CFS and FM
https://www.healthrising.org
Hunter-Hopkins Center
https://drlapp.com/
International Association for CFS and ME
http://iacfsme.org/
Invest in ME Research Colloquium/Conference Site
www.investinme.org
Jennifer Brea
http://www.jenniferbrea.com
Mast Cell Action
https://www.mastcellaction.org/about-mcas
ME Action Network
https://www.meaction.net/
ME Association – United Kingdom
https://www.meassociation.org.uk/
ME/CFS Research Review
https://mecfsresearchreview.me/
National CFIDS Foundation
http://www.ncf-net.org/whatisCFIDS.htm
National Fibromyalgia Association
http://www.fmaware.org/
Naviaux Lab – Dr. Robert Naviaux (MD, PhD)
http://naviauxlab.ucsd.edu/science-item/chronic-fatigue-syndrome-research/
Neurally Mediated Hypotension – patient brochure
http://www.njcfsa.org/wp-content/uploads/2010/08/4-11-Patient-Unofrmationon-Neurally-Mediated-Hypotension-and-its-Treatment.pdf
Open Medicine Foundation
https://www.omf.ngo/
https://www.omf.ngo/collaborative-research-center-harvard/
Science for ME – Where Science and the ME/CFS Community Meet
https://www.s4me.info/
Sjogren’s Syndrome Foundation
https://www.sjogrens.org/home/about-sjogrens
Solve ME/CFS Initiative
https://solvecfs.org
https://solvecfs.org/announcing-smcis-new-mecfs-research-program-at-brighams-and-women-hospital/
Stanford Medicine ME/CFS Initiative
http://med.stanford.edu/chronicfatiguesyndrome/research.html
The Microbe Discovery Project
http://microbediscovery.org/
The Optimum Health Clinic Foundation
https://www.theoptimumhealthclinic.com/
The York ME Community
http://www.york-me-community.org/video/
Whittemore Peterson Institute
http://nvcbr.org/2016/05/11/myalgic-encephalomyelitis/