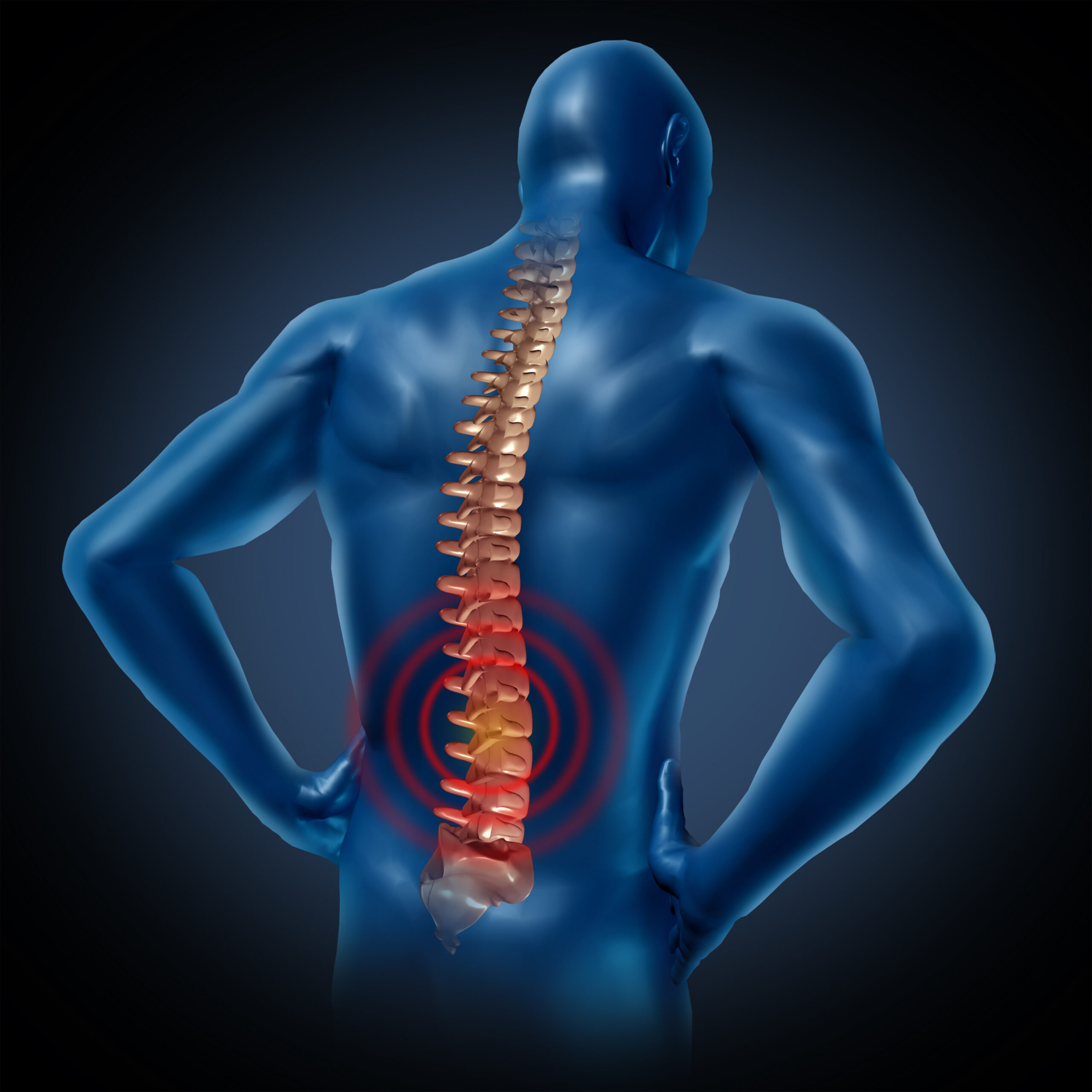
When and how is spinal decompression therapy used?
Spinal decompression therapy is used for relieving back pain caused by bulging or herniated discs, as well as for treating conditions like sciatica, degenerative disc disease, radiculopathy (diseased spinal nerve root) or worn spinal joints.
The procedure can be performed both invasively and non-invasively, the former involving surgical decompression, while the latter consists in stretching the spine using only external tools.
The treatment can be associated with other procedures that are thought to be effective in relieving the pressure exerted on the spinal nerves. Such solutions include electrical stimulation, head or cold therapy, ultrasound therapy and even whole body vibration therapy.
How spinal decompression works
In a typical non-surgical spinal decompression therapy session, the patient lies in a prone position (face down) on a computer-controlled table, with a harness fitted around the pelvis and another one around the trunk. This mechanical traction device is controlled by the physician who operates the computed, and allows one to vary the force and angle so as to reposition the spine and take the pressure off the discs.
Spinal decompression is different from traction; traction consists in applying a force along the spine in order to elongate it and stretch the muscles and joints. Although effective in some patients, traction produces little to no effect in others, so it’s not always a good solution for achieving pain relief.
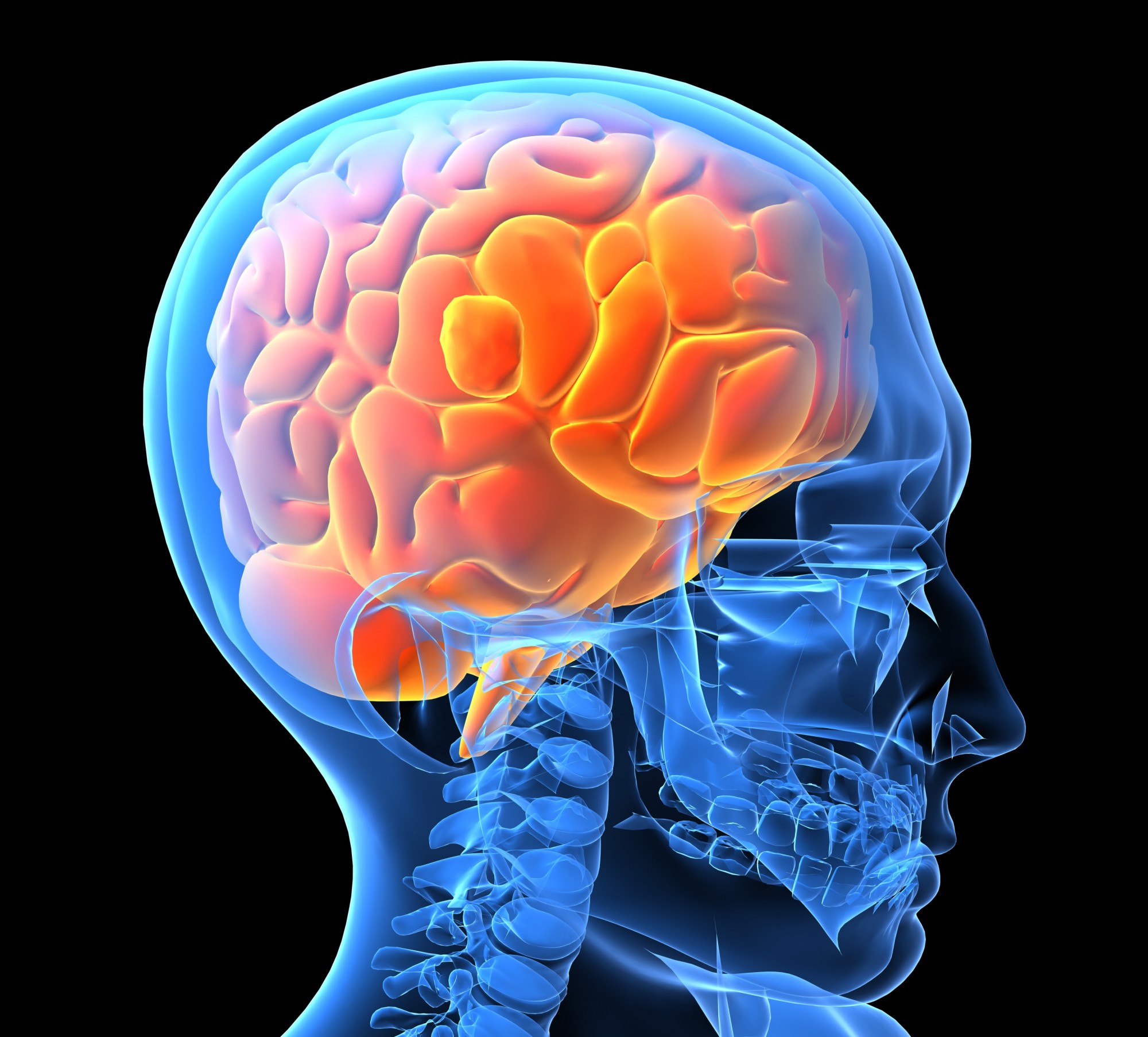
Decompression on the other hand has been shown to be more efficient and to cause no side effects. Some chiropractors and physicians say that spinal decompression is more effective because it addresses the root cause of the problem, while traction only addresses the effects. During decompression, thanks to the computer-powered tools, the muscular reaction is monitored throughout the procedure and the direction and intensity of the force can be adjusted to target a specific segment of the spine.
A typical therapy session lasts between 30 and 45 minutes, and one may need to undergo up to 7 weeks of treatment (20-28 interventions), depending on the severity of their condition. Proponents of spinal decompression say that the pressure applied during this treatment causes the herniated and bulging discs to retract in time, and promotes the blood flow to the spine, leading to a better delivery of nutrients, oxygen and water and thus speeding up the recovery.
When is spinal decompression needed?
Spinal decompression is used in facet syndrome, sciatica, chronic and acute neck or low back pain, disc herniation, degenerative disc disease and spinal stenosis.
As a general rule, patients who suffer from recurrent pain from back surgery, from degenerated discs that don’t respond to conventional therapy, as well as those with herniated and lumbar discs that are more than 4 weeks old are good candidates for spinal decompression. There are, however, some categories of patients who shouldn’t undergo this procedure.
Exclusion criteria for spinal decompression include patients with spinal fusions with metallic roods, people with severe osteoporosis or lumbar vertebral compression fracture below L1, people with aneurysms, spinal osteomyelitis or meningitis. Patients with severe peripheral neuropathy, those with cauda equina syndrome, people with unstable spondylolisthesis as well as pregnant women should not rely on spinal decompression.
The procedure is safe and comfortable, and helps in decreasing the pain and improving the function of the spine. It can also improve one’s posture and quality of life by allowing them to perform daily activities without experiencing pain and discomfort.
Although some are still reluctant to this form of therapy, there are several studies that support the use of spinal decompression in patients with lumbosacral pain, disc herniation and other such conditions.
Have something to add to this article? Feel free to comment below or join our Facebook community and share your thoughts with us!
References:
Apfel C., Cakmakkaya O., Martin W. et al. – Restoration of disk height through non-surgical spinal decompression is associated with decreased discogenic low back pain: a retrospective cohort study, BMC Musculoskeletal Disorders, 2010, 11:155
Thomas G., Groteke E. – Surgical Alternatives: Spinal Decompression, Orthopedic Technology Review, 2003, 6(5)
Shealy N., Borgmeyer V. – Decompression, Reduction and Stabilization of the Lumbar Spine: A Cost-Effective Treatment for Lumbosacral Pain, American Journal of Pain Management, 1997, 7(2)
Grose E., Naguszewski W., Naguszewski R. – Vertebral axial decompression therapy for pain associated with herniated discs or facet syndrome: An outcome study, Journal of Neurological Research, 1998, 20:186-90