With type 2 diabetes, complications ca easily occur if you don’t do your best to keep blood glucose levels under control. Some of these consequences are short-term, for example the rise of glycemia levels after a meal, followed by hypoglycemia (very low blood glucose), while others are long-term and can severely affect your health and quality of life.
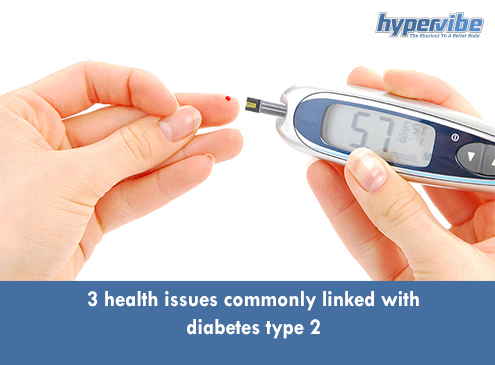
Everybody knows that diabetes type 2 develops when the body can’t process blood sugar efficiently, due to insufficient insulin production, or to an improper use of existing insulin. The result is high blood sugar levels, which can be easily detected with a glucose meter at home, by putting a drop of blood on a test strip and waiting about 15 seconds for the glycemia values to be displayed.
This is what we know diabetes does to our body, but it’s only one of the ways this condition affects our health. So let’s take a look at four other potential consequences of high blood sugar levels and health issues linked with diabetes type 2.
Diabetes is a condition that develops gradually so you may not realize that you have high blood sugar levels for some time, but the unbalanced glycemia levels affect your body and cause damage over time. One of the consequences that may remain unnoticed for a while is inflammation, which has been found to play a role in the development of type 2 diabetes, and can be the trigger of other unwanted complications.
In diabetes patients, inflammation is internal. Insulin controls not only the levels of blood sugar, but also the accumulation of fat around the waist area and on major internal organs, and when there are too many fat cells, they can produce chemicals that favor inflammation.
Levels of cytokines for example are higher in people with type 2 diabetes than in healthy adults, and researchers have found that these chemicals are elevated especially inside the fat tissue. Scientists concluded that excess body fat, especially in the abdominal area, favors the production of inflammation-inducing cells, making one more prone to a variety of ailments. Insulin resistance, which is present in diabetes patients, also favors inflammation.
A recent study found that people who work shift hours are more prone to metabolic diseases like type 2 diabetes because of the altered production of sleep hormone melatonin. Increased levels of this hormone reduce the ability of insulin-producing cells to release insulin, making on more prone to hyperglicemia and more prone to developing diabetes type 2.
Melatonin is involved in maintaining the normal circadian rhythm or day-night cycle by regulating other hormones, and the production of this substance varies during the day, being higher at night and lower in the morning.
The mentioned study tested the insulin and melatonin levels of 45 healthy participants with the same body mass index, and no differences in family history of diabetes, and treated them with 4 mg of melatonin every day, for 3 months. At the start and end of the treatment period their blood sugar and insulin levels were compared and results showed that participants had higher levels of blood sugar and lower production of insulin after taking melatonin.
Other potential sleep problems linked with diabetes type 2 include restless leg syndrome and obstructive sleep apnea.
Diabetes type 2 affects the tiny blood vessels that feed the feet and the nerves in the lower body, and can lead to pain and cramps, weakness, a tingling sensation in the limbs and a high risk of developing diabetes neuropathy.
In patients with diabetic neuropathy, nerves are damaged, so they’re not able to feel or notice injuries. Blisters, sores and other injuries can remain unnoticed for a while, and this favors the development of infections and the occurrence of more serious complications. The infection can spread faster in people who don’t have proper feet hygiene, in those who wear shoes that fit poorly, as well as in people who spend a lot of time standing or sitting, as this can affect the circulation and nerves even more.
Diabetic neuropathy appears due to nerve damage caused by hyperglycemia, and is one of the severe complications that can be recognized without a special test, as it manifests through persistent sores, dry and cracked skin, calluses, cold feet that result from poor circulation, and infected ulcers that can lead to gangrene and the need for amputation. About 1 in 10 patients with diabetes gets feet ulcers.
Type 2 diabetes is commonly associated with a series of short- and long-term complications, but if you watch your diet and sleep schedule and stay active, you can maintain good blood glucose control and avoid these unwanted effects.
Have something to add to this article? Comment below or join our Facebook community and share your thoughts with us!

Updated on: 08.09.2021 The lymphatic system is involved not only...

Stress can make you gain weight – we’ve heard this...
Various theories exist to answer this question. As you will...

Both rebounding and jumping on a trampoline are excellent ways...

Our series of whole body vibration machine exercise articles continues...