5 Conditions that Can Cause Bone Loss

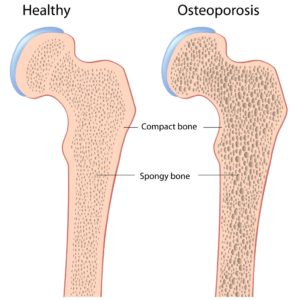
People over 50 are more likely to develop osteoporosis and to break a bone, aging being one of the factors that contributes to bone loss. For women, menopause comes with a drop in estrogen levels, which is a major trigger for bone loss, and for men, a decrease in the production of testosterone also favors the loss of bone mass.
These changes can make one more prone to fractures, but it’s not a must for one to develop osteoporosis. The human body produces new bone tissue and reabsorbs the old one on a continuous basis, as we grow up and age. As long as a balanced diet is maintained and the mineral intake is adequate, especially the intake of calcium and phosphate, one can maintain healthy and strong bones.
Practicing strength exercises also helps in stimulating bone mass production and in increasing density, but some unhealthy habits, like drinking alcohol or smoking can lead to weaker bones. Also, in young women, heavy and long menstrual periods can accelerate the loss of bone mass, and lead to fragile and brittle bones.
Besides these factors, there are also long-term medical conditions that favor the weakening of bones, and 5 of these conditions will be addressed in this article.
1. Diabetes
People suffering from type 1 diabetes seem to be more prone to developing osteoporosis and to losing bone mass, although the reasons aren’t fully understood. It’s been shown that in patients affected by this condition, the bone turnover is lower, therefore the tissue forms slower but the loss of mass due to bone reabsorption doesn’t happen slower.
Those with type 2 diabetes are also at higher risk of developing osteoporosis and breaking a bone, scientists agreeing that high blood sugar levels affect the formation of new bone mass. Both men and women affected by diabetes can suffer from low bone density; along with the occasional hypoglycemic episodes and with the poor sensation in feet due to neuropathy, the fragile bones can increase the risk of falls and fractures.
2. Chronic kidney or liver disease
People with chronic kidney disease often follow medical treatments based on glucocorticoids, medications that put them at higher risk for developing osteoporosis. Moreover, these individuals are more likely to develop metabolic bone diseases that affect the formation of new bone tissue and lead to vitamin D deficiency, therefore to an impaired absorption of calcium as well.
Patients suffering from chronic liver disease are also more likely to break a bone or suffer from osteoporosis, as vitamin D deficiency and a poorer absorption of calcium are typical for liver disease. Bone formation in these people is reduced, and if they’re treated with medications like prednisone, chronic liver disease sufferers can experience even greater bone loss.
3. Celiac disease and malabsorption syndromes
Chron’s disease, celiac disease and ulcerative colitis can all favor malabsorption, leading to lower than normal levels of vitamin D and calcium and as a result to an increased risk of developing osteoporosis. Bones tend to be weaker and more fragile in people suffering from bowel diseases, as the body absorbs fewer nutrients from foods and the bone cells can be deprived from important minerals and vitamins.
Celiac disease and gluten allergy or sensitivity in non-celiacs can interfere with the digestion of nutrients, as the lining of the digestive system gets damaged. In such conditions, even if the celiac sufferer gets enough calcium or vitamin D from food, their digestive system may not be able to properly process the nutrients and the bone density can decrease.
4. Rheumatoid arthritis
An autoimmune disorder, rheumatoid arthritis causes the inflammation of the joints, so it can put one at higher risk for developing osteoporosis, just like any other chronic inflammatory disease. In RA, the body attacks its own cells, destroying the healthy tissue, so it’s not hard to guess why this condition can make one more prone to fractures and can weaken their bones.
Given that the bone turnover rate is affected, old bone is replaced with new tissue in an unbalanced manner, and if the patient takes corticosteroids to relieve the symptoms of rheumatoid arthritis, the risk of osteoporosis becomes even greater. Not to mention that arthritis, regardless of its form, causes pain and discomfort and often leads to inactivity. The lack of physical activity and strength exercises can favor the loss of bone mass, resulting in poor balance and an increased risk of fractures due to falls.
As for medication, it’s known that long-term use of steroids leads to osteoporosis, and RA patients are susceptible to this disorder. Also, those affected by lupus are more likely to suffer from abnormal bone loss, as this condition impedes the growth of bone tissue.
5. Hyperthyroidism
An overactive thyroid gland means a higher production of thyroid hormone, which seems to increase the number of bone-remodeling cycles, causing your body to lose more bone tissue that it produces. This alteration in the bone formation / reabsorption ratio makes one more prone to breaking a bone and developing osteoporosis.
When there’s too much thyroid hormone inside the body, the calcium absorption is affected therefore the bones no longer receive the needed amount of minerals. This contributes to bone tissue loss and over time to osteoporosis, falls and fractures.
Besides these conditions, some neurological disorders are also associated with a higher risk of falls and broken bones. Spinal cord injuries for example or other conditions that affect one mobility and require bed rest for prolonged intervals can favor bone loss.
Have something to add to this article? Comment below or join our Facebook community and share your thoughts with us!